General Questions
What happens during my first visit?
During your first visit you can expect the following:
- Arrive at your appointment with your paperwork completed (you can download it from our website – see the paperwork link).
- You will provide us with your prescription for occupational therapy.
- We will copy your insurance card.
- You will be seen for the initial evaluation by the therapist.
- The therapist will discuss the following:
- Your medical history.
- Your current problems/complaints.
- Pain intensity, what aggravates and eases the problem.
- How this is impacting your daily activities or your functional limitations.
- Your goals with occupational therapy.
- Medications, tests, and procedures related to your health.
- The therapist will then perform the objective evaluation which may include some of the following:
- Palpation – touching around the area of the pain/problem. This is done to check for the presence of tenderness, swelling, soft tissue integrity, tissue temperature, inflammation, etc.
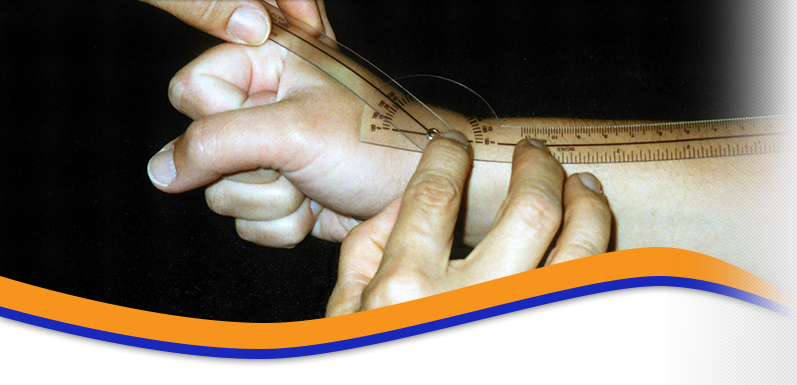
- Range of Motion (ROM) – the therapist will move the joint(s) to check for the quality of movement and any restrictions.
- Grip & pinch strength and/or Muscle Testing – the therapist may check for strength and the quality of the muscle contraction. Pain and weakness may be noted. Often the muscle strength is graded. This is also part of a neurological screening.
- Neurological Screening – the therapist may check to see how the nerves are communicating with the muscles, sensing touch, pain, vibration, or temperature. Reflexes may be assessed as well
- Special Tests – the therapist may perform special tests to confirm/rule out the presence of additional problems.
The therapist will then formulate a list of problems you are having, and how to treat those problems. A plan is subsequently developed with the patient’s input. This includes how many times you should see the therapist per week, how many weeks you will need therapy, home programs, patient education, short-term/long-term goals, and what is expected after discharge from therapy. This plan is created with input from you, your therapist, and your doctor.
What do I need to bring with me?
Make sure you bring your occupational therapy referral (provided to you by your doctor) and your payment information. If your insurance is covering the cost of occupational therapy, bring your insurance card. If you are covered by Workers’ Compensation, bring your claim number and your case manager’s contact information. If you are covered by auto insurance or an attorney lien, make sure you bring this information.
How should I dress?
You should wear loose fitting clothing so you can expose the area that we will be evaluating and treating. For example for a shoulder problem, a tank top is a good choice, so we can perform a thorough examination.
How long will each treatment last?
Treatment sessions typically last 30 to 60 minutes per visit
How many visits will I need?
This is highly variable. You may need one visit or you may need months of care. It depends on your diagnosis, the severity of your impairments, your past medical history, etc. You will be re-evaluated on a monthly basis and when you see your doctor, we will provide you with a progress report with our recommendations.
Is occupational therapy painful?
For many patients, one of the primary objectives is pain relief. This is frequently accomplished with hands-on techniques, modalities such as ultrasound, electrical stimulation, and/or heat or cold therapy. Movement often provides pain relief as well. Your occupational therapist will provide you with the appropriate exercises not only for pain relief but to recover range of motion, strength, and endurance.
In some cases, occupational therapy techniques can be painful. For example, recovering wrist range of motion after wrist surgery may be painful. Your occupational therapist will utilize a variety of techniques to help maximize your treatment goals. It is important that you communicate the intensity, frequency, and duration of pain to your therapist. Without this information, it is difficult for the therapist to adjust your treatment plan.
Who pays for the treatment?
In most cases, health insurance will cover your treatment. Click on our insurance link above for a summary of insurances we accept and make sure you talk to our receptionist so we can help you clarify your insurance coverage.
What types of treatments will I receive?
There are dozens of different types of treatment interventions. Here is a list of treatment interventions:
- Active Range of Motion (AROM) – the patient lifts or moves a body part through range of motion against gravity. AROM is usually one of the first modalities prescribed for arthritis.
- Active Assistive Range of Motion (AAROM) – therapist-assisted active range of motion. This is usually prescribed for gentle stretching or strengthening for a very weak body part.
- Isometrics – muscle contraction without joint movement. This is usually prescribed for strengthening without stressing or damaging the joint (e.g., arthritis, or exercises to be performed in a cast, or right after surgery if recommended by the therapist/doctor).
- Isotonics – muscle(s) contracting through the ROM with resistance. This is usually prescribed for strengthening.
- Soft Tissue Mobilization – therapeutic massage of body tissue performed with the hands. Soft tissue mobilization may be used for muscle relaxation, to decrease swelling, to decrease scar tissue adhesions, and for pain relief.
- Mobilization – hands-on therapeutic procedures intended to increase soft tissue or joint mobility. Mobilization is usually prescribed to increase mobility, delaying progressive stiffness, and to relieve pain. There are many types of mobilization techniques including Maitland, Kaltenborn, Isometric Mobilizations, etc.
- Proprioceptive Neuromuscular Facilitation (PNF) – a system of manually resisted exercises performed in diagonal patterns that mimic functional movements. PNF was initially used in developmentally and neurologically impaired patients but now is used in almost every aspect of neuromuscular retraining from athletes in sports facilities to the very weak in hospitals and nursing homes.
- Progressive Resistive Exercises (PRE) – exercises that gradually increase in resistance (weights) and in repetitions. PRE is usually prescribed for reeducation of muscles and strengthening. Weights, rubber bands, and body weight can be used as resistance.
- Passive Range of Motion (PROM) – the patient or therapist moves the body part through a range of motion without the use of the muscles that “actively” move the joint(s).
- Stretching/Flexibility Exercise – exercise designed to lengthen muscle(s) or soft tissue. Stretching exercises are usually prescribed to improve the flexibility of muscles that have tightened due to disuse or in compensation to pain, spasm or immobilization.
- Cryotherapy or Cold Therapy – used to cause vasoconstriction (the blood vessels constrict or decrease their diameter) to reduce the amount of fluid that leaks out of the capillaries into the tissue spaces (swelling) in response to injury of tissue. Ice or cold is used most frequently in acute injuries, but also an effective pain reliever for even the most chronic pain.
- Neuromuscular Electrical Stimulation (NMES) – the application of electrical stimulation to aid in improving strength (e.g., the quadriceps muscle after knee surgery or injury). NMES is also used to decrease pain and swelling and to relieve muscle spasm.
- Heat – heat is recommended to decrease chronic pain, relax muscles, and for pain relief. It should not be used with an acute or “new” injury.
- Iontophoresis – medications are propelled through the skin by an electrical charge. This modality works on the physical concept that like charges repel each other, therefore, a positively charged medication will be repelled through the skin to the underlying tissues by the positively charged pad of an iontophoresis machine. Iontophoresis is usually prescribed for injuries such as shoulder or elbow bursitis.
- Transcutaneous Electrical Nerve Stimulation (TENS) – a relatively low voltage applied over painful areas through small self-adhesive electrodes. The electrical stimulation “disguises” or “overrides” the sensation of pain. It is a small, portable unit, used in intervals, to control pain and reduce dependence on drugs. It is usually prescribed for relief of pain.
- Ultrasound – ultrasound uses a high frequency sound wave emitted from the sound head when electricity is passed through a quartz crystal. The sound waves cause the vibration of water molecules deep within tissue causing a heating effect. When the sound waves are pulsed, they cause a vibration of the tissue rather than heating. The stream of sound waves helps with nutrition exchange at the cellular level and healing. Studies have shown that ultrasound is helpful for ligament healing and clinically, for carpal tunnel syndrome, and muscle spasm.
- Whirlpool – immersion of a body part into water with small “agitators” to provide a gentle massaging motion. A warm whirlpool provides relief from pain and muscle spasm and is often preparatory to stretching or exercise. Cold whirlpool is used to decrease inflammation and swelling. Whirlpool may also be used for wound care following surgery.
How does the billing process work?
Billing for occupational therapy services is similar to what happens at your doctor’s office. When you are seen for treatment, the following occurs:
- The occupational therapist bills your insurance company, Workers’ Comp, or charges you based on Common Procedure Terminology (CPT) codes.
- Those codes are transferred to a billing form that is either mailed or electronically communicated to the payer.
- The payer processes this information and makes payments according to an agreed upon fee schedule.
- An Explanation of Benefits (EOB) is generated and sent to the patient and the occupational therapy clinic with a check for payment and a balance due by the patient.
- The patient is expected to make the payment on the balance if any.
It is important to understand that there are many small steps (beyond the outline provided above) within the process. Exceptions are common to the above example as well. At any time along the way, information may be missing, miscommunicated, or misunderstood. This can delay the payment process. While it is common for the payment process to be completed in 60 days or less, it is not uncommon for the occupational therapy clinic to receive payment as long as six months after the treatment date
What is your privacy policy?
Our privacy policy can be read here: Notice of Privacy Practices.
Carpal Tunnel Syndrome
What is Carpal Tunnel Syndrome?
Carpal tunnel syndrome is a disorder that causes pain, weakness and numbness in the hand and wrist. Patients often complain of symptoms during activities such as driving a car, holding a telephone, and reading the newspaper. It occurs due to increased pressure on the median nerve at the wrist. The associated pain occurs most often on the palm side of the wrist and hand but may be diffuse. The pain may radiate to the forearm and shoulder but rarely to the neck.
The median nerve provides sensation to the thumb, index, long and half the ring fingers; therefore, patients with carpal tunnel syndrome will classically feel numbness and tingling in this distribution. Some patients may feel numbness about the entire hand. These symptoms may occur with activities during the day or while at rest during the night. In addition to numbness and pain, patients may complain of weakness of the hand and dropping objects. With a more severe carpal tunnel syndrome, atrophy of the muscles at the base of the thumb may be noted.
What is the carpal tunnel?
There are eight carpal bones of varying shape and size that make up the wrist. These carpal bones form a C-shaped ring that is covered by a ligament, the transverse carpal ligament. The ligament and bones form the carpal tunnel through which pass the median nerve and nine tendons that flex the fingers and thumb. Any condition that decreases the size of the tunnel or increases the size of the contents can cause carpal tunnel syndrome.
What causes carpal tunnel syndrome?
There are numerous factors that may cause carpal tunnel syndrome. It may be related to strenuous repetitive use of the hands or occur after trauma such as a wrist fracture. The nerve can be compressed from something extra within the canal. This includes a mass, an anomalous muscle, or a hematoma which can occur particularly in patients taking anticoagulation medication after a fall on the hand. Other disorders associated with carpal tunnel syndrome include but not limited to: pregnancy, diabetes mellitus, hypothyroidism, alcoholism, severe infections, arthritic diseases, and gout.
How does the doctor make the diagnosis of carpal syndrome?
The physician can often make the diagnosis after the patient has explained their symptoms and the extremity has been examined. During the examination, the physician may perform certain provocative maneuvers to determine if carpal tunnel syndrome is evident. By tapping over the nerve at the wrist, termed Tinel’s sign, a patient with carpal tunnel syndrome may note a tingling sensation in the digits innervated by the median nerve. Similar findings may be noted while holding the wrist fully flexed or extended, termed Phalen’s and reverse Phalen’s signs. The strength of the muscles of the hand are evaluated as well as the sensation. An EMG / NCV, electromyography and nerve conduction velocity, is often performed to confirm the diagnosis and determine severity. Xrays are not routinely obtained.
How is carpal tunnel syndrome treated?
Patients with carpal tunnel syndrome due to a specific medical condition such as diabetes or a thyroid disorder should have the associated medical disorder treated appropriately. Wrist splints are used at night and during the day during activities that may exacerbate the symptoms. Non-steroidal anti-inflammatory medications may be of benefit but have the risk of gastritis. Alteration of activities is important. This includes taking frequent breaks from repetitive activities, and stretching before and after activities. A hand therapist may be helpful with providing ergonomic tips or performing a work place evaluation. A corticosteroid injection of the carpal canal often provides temporary relief. Approximately 25% of patient treated with an injection will have long-term relief of their symptoms. Non-operative treatment modalities from a hand therapist may be performed for several months; however, if the symptoms persist or progress surgical treatment is considered. Those patients with a severe carpal tunnel syndrome are considered for surgery more promptly since the non-operative modalities typically are not helpful at this stage.
What is involved in the surgery for carpal tunnel syndrome?
Carpal tunnel release is the most common procedure performed in the upper extremity. In general surgical procedures for carpal tunnel syndrome, the transverse ligament is cut over the canal to take the pressure off the median nerve. The surgery is performed on an outpatient basis under local anesthesia and often in conjunction with intravenous sedation. The procedure may be performed using the open technique in which an incision is made in the palm to cut the ligament. The nerve and canal is inspected to confirm that there is no other process compressing the nerve. The skin is sutured and a sterile dressing and often a splint are applied. The sutures are removed in 10 – 14 days and a custom developed exercise program with a hand therapist in started.
An alternative surgical procedure is the endoscopic carpal tunnel release in which one or two smaller incisions are made at the palm and or wrist and the ligament is cut while keeping the skin above the ligament intact. The benefit of the endoscopic release is less postoperative pain, earlier return of grip strength, and earlier return to work.
What are the results of surgery for carpal tunnel syndrome?
The majority of patients undergoing carpal tunnel release note an improvement in their symptoms. Some patients may notice persistent numbness and tingling. This will occur particularly in patients that have a more severe carpal tunnel syndrome. At this stage more permanent changes may have occurred within the nerve due to longstanding compression. Other patients may notice persistent or recurrent symptoms due to other factors for example nerve compression in the neck (cervical radiculopathy), or a polyneuropathy due to diabetes. Most patients are capable of performing their activities of daily living soon after the procedure. Pain about the about the palm is often noted initially that is treated with scar massage. This scar pain is one reason full grip strength often does not return until three months after the procedure.
What are the risks of surgery for carpal tunnel syndrome?
There is a small risk of nerve injury since the procedure is performed adjacent to the nerve. The endoscopic release has a higher risk of nerve and blood vessel injury as compared to the open procedure. There is a low risk of infection and bleeding during the procedure is minimal. Hand and wrist stiffness is a potential risk but is uncommon if the postoperative exercises are performed.
Dupuytren’s Contracture
What is Dupuytren’s Contracture?
Dupuytren’s contracture, also known as Dupuytren’s disease, refers to the formation of thick “scar-like” tissue on the palm extending to any finger. This leads to a contracture of the involved finger, such that the patient cannot extend the finger fully because of the tethering effect of the thick “scar-like” tissue located on the palm. Dupuytren’s contracture can involve one or many fingers of the same hand.
What causes Dupuytren’s Contracture?
The exact causes of Dupuytren’s Contracture are not yet known, although it may be genetically linked. Current research suggests a problem with inflammation in the palm of the hand leading to the formation of thick “scar-like” bands.
Is there any cause and effect relationship between Dupuytren’s Contracture and other diseases?
Patients with diabetes have been known to develop a form of Dupuytren’s Contracture that is less severe than the regular form. There have also been studies linking alcoholism and tobacco use to Dupuytren’s Contracture, but these studies have not been verified.
What are the typical symptoms?
When a thick “scar-like” band forms a puckering appearance along the palm of the hand and extends onto a finger, the finger begins to flex inwards towards the palm. The patient will then be unable to fully extend the finger either actively or passively. This flexion is usually progressive and if left untreated the patient will lose the ability to fully straighten the fingers.
How can it be treated?
Once the “scar-like” band has begun to form and the finger flexion is progressive, surgery is the best option.
If surgery is an option, how is it performed?
Surgery is performed by making an incision in the palm of the hand and in the involved finger. The thick “scar-like” band is then removed and the finger is extended. The hand is then splinted for 3-5 days for comfort and hand therapy involving active range-of-motion exercises is initiated 3 days after surgery. The hand therapist will fabricate a custom extension hand splint that is worn at night for several months to prevent recurrent contracture. Returning to everyday and occupational activities is encouraged at the earliest opportunity.
What are the chances of success?
Dupuytren’s Contracture is a very difficult problem to treat. Five to ten years after surgery, the possibility of recurrence has been found to be as high as 50%. The possibility of recurrence depends not only on the surgery but also on the rehabilitation program following surgery and on the motivation of the patient.
What are the possible complications of surgery?
Each finger has two nerves and two arteries running along the side of the finger. Damage to either one of the nerves and/or one of the arteries of the involved finger is possible. If a nerve is injured, it can be repaired but a portion of the finger may become numb until the nerve has healed. If one of the arteries is injured, then repair is not always necessary because the other artery can provide sufficient blood flow to the finger. Skin loss over the area of the incision can also occur but is relatively unusual. If this were to happen a skin graft may be required.
What would happen in the long run if I receive no treatment?
If the Dupuytren’s Contracture is not treated surgically, then the involved finger(s) will progressively become more flexed and eventually the patient will not be able to extend the finger at all. Simple everyday activities may become difficult such as shaking hands, washing your hands and/or grasping/releasing objects. If many fingers are involved, loss of function of the entire hand may occur.
Mallet Finger
What is a mallet finger?
It is a deformity caused by rupture of the tendon at the tip of the finger. This can also occur with a fracture.
What does a mallet finger look like?
It is a finger that is bent at the tip and one cannot make it straight.
Can it get worse if it goes untreated?
It can stay the same or get worse.
Does it need surgery?
If the finger is bleeding or has an open wound it should be treated immediately. If there is a fracture that is large or out of position it may need surgery. If there is no fracture, splinting the finger in a straight position may be all that is necessary but it must be properly evaluated by a hand surgeon to make sure there are no additional problems.
What type of doctor treats a mallet finger?
A hand surgeon, an orthopaedic, plastic or general surgeon that specializes in hand injuries, is most helpful. He or she may refer you to a hand therapist for custom splinting and monitoring the condition.
How long does the splint have to stay on?
Will the finger be stiff after the splinting period?
The finger will regain movement very gradually. It should not be forced because mallet deformity could reoccur. The hand surgeon may send you to a hand therapist to be instructed in proper care and exercises.
Will the finger look normal after the injury?
The tip of the finger may remain slightly thicker. There may also be a slight loss in movement, that is, it may not be fully straight or may not bend fully. However, most mallet injuries recover full function.
Is there a lot of pain?
When the injury is to the tendon, there may be no pain. Some people do experience pain if there is a fracture. During the splinting process the pain is minimal. Once hand therapy or exercises begin, there may be some discomfort with movement initially but this is usally resolved with continued gentle exercises.